I’ll admit, as an activist, I’m often in fight the system mode. I approach even do-gooders with defensiveness. Why?
Because trauma survivors have not been invited to the table for decades even when it’s to have a conversation about what trauma survivors need.
We need a lot because we’ve been through a lot. Many of us have had little in the way of compassionate and competent care that is affordable, accessible or appealing.
I often go into conversations or talks needing to make one or all of the following points:
- Adverse Childhood Experiences (ACEs) have long-term consequences.
- Developmental trauma impacts adults even after childhood has ended.
- Trauma survivors know best which treatments do and don’t work, what our 24/7 needs are in and outside of clinical settings and how to speak for ourselves about our past and present experiences.
These ideas are obvious to some but seem radical to others. I’ve been to a3-day conference in Boston on trauma, traumatic stress and treatment effectiveness where :
- Trauma survivors were referred to as “them” rather than “us”
- ACEs were mentioned once in passing
- Not one self-identified trauma survivor spoke as panelist, presenter, guest or was even represented as a vendor.
- Where trauma survivors are referred to only as patients not parents, professionals or people.
The Partnering for Excellence (PFE) conference, held last month in North Carolina was different. Shockingly different. It was a conference that walked the trauma-informed talk.
 PFE is an initiative started in 2012 which and is described as seeking to “strengthen public-private partnerships in child welfare to enhance quality of care and significantly improve child functioning and well-being outcomes.” That’s the description given in the bio of the Project Director, Jenny Rahilly Cooper.
PFE is an initiative started in 2012 which and is described as seeking to “strengthen public-private partnerships in child welfare to enhance quality of care and significantly improve child functioning and well-being outcomes.” That’s the description given in the bio of the Project Director, Jenny Rahilly Cooper.
Cooper herself described the overarching goal of PFE more spefically at the conference as follows:
“To Redesign how the Child Welfare and Child Mental Health systems interact so they can:
Provide trauma informed services and improve family outcomes
Reduce high-end services
Prevent children from being taken in to DSS custody.”
PFE is funded by Benchmarks: An Alliance of Agencies Helping Children, Adults & Families, located in North Carolina. Benchmarks is sponsoring the project investigators, Katie Rosanbalm and Christina Christopoulous, who are from the Center for Child and Family Policy at Duke University.
Rosanbalm and Cooper presented at the conference to an audience of about 150 people from the Department of Social Services (DSS), managed care mental health organizations, various advocacy groups as well as trauma survivors who have used “the system” being discussed.
The PFE model is being piloted on a county level, so far, and the two most important parts of the program, in my view, are these:
- The focus on training all who come into contact with kids referred to DSS about trauma’s impact and the evidence-based treatments for trauma (another article will someday be about if evidence-based and effective are the same).
- The length, depth and type of screening now done when children have been referred to DSS. Instead of one 50-minute assessment, as those referred to DSS, through the PFE counties, get a Trauma Informed Comprehensive Checklist Assessment (called a “TICCA”) which is much more thorough.
- Children spend three to five (it sounds more like three) hours with birth or foster family as well as a social worker and mental health provider.
- The mental health provider must use the TICCA and has become trauma-informed.
Assessments are done in a trauma-informed way and those who work with kids and families understand trauma, trauma symptoms and trauma treatment.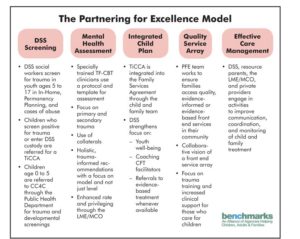
This is huge when one considers this fact:
“Among children in DSS custody, every single one (100%) has screened positive for trauma (Benchmarks, 2016)” as reported here. At the conference, many of us learned about the PFE model.
An understanding of trauma and ACEs are essential, not optional or an after thought.
This was evident even at the conference about the PFE model.
Everyone had a seat at the same table. Literally. We actually sat three people to a table at the conference. Together, we listened and learned.
Many of us spent the previous night watching the Paper Tigers documentary and having a panel discussion afterwards. This is a must-see, not optional movie for anyone who cares about kids or trauma. Period.
The goal of a TICCA is not soley to remove children from specific situations which have been and maybe are traumatic but also to assess the needs of children (and in turn, their families) in order to make short AND long-term placement and treatment plans.
It’s clear that there are large parts of “the system” that need improvement, in North Carolina, as elsewhere.
The system, like the family unit, is meant to serve and protect and nurture children and families.
The system, like the families, sometimes operates in ways that traumatize, injure and neglect. Rarely, is this intentional. Hardly ever is anyone motivated by the desire to do harm. There’s room for improvement at all levels.
This was acknowledged and discussed and that’s so rare and impressive.
Many families have had multi-generational involvement with DSS and the mental health system and those interactions have not always beneficial or trauma-informed.
As is the case in many states, local DSS offices often work as independent units rather than as a larger and more cohesive whole. This is obviously problematic but especially so since children move often, are placed repeatedly and therefore end up in different schools, homes, shelters, offices, treatment facilities and with different caregivers, providers and people in their lives (as in, not all that trauma-informed).
Information does not always get shared or services may be halted or interrupted or made inaccessible (as in, not terribly effective). 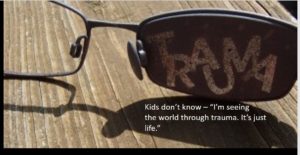
PFE is an ambitious program but it’s necessary and if it’s effective, will do what most everyone wants. Protect kids. Support families. Save money.
The effectiveness of the program is still be assessed and analyzed but there is one notable development worth reporting.
The number of children being diagnosed with post-traumatic stress disorder has increased while the number of children being diagnosed as psychotic and/or with ADHD, conduct disorder or other labels is decreasing. See these slides from a Children’s Services Practice Notes post.
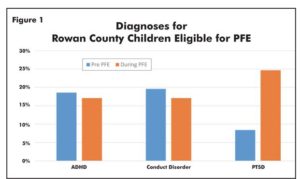
This is important for many reasons.
- It not impacts the treatment and medications a child may be prescribed.
- It flags the trauma as the problem and not the child or the child’s symptoms.
- It encourages those who work with the child, teachers, school administrators, nurses and foster families to learn about trauma (yes!).
- It encourages more understanding and compassion and less stigma and shame.
- It not only means a child is getting a more accurate diagnosis and better treatment but being medications and treatment for conditions they do not and maybe never did even have. HUGE!
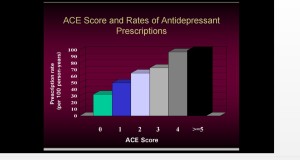
Sometimes we can all forget that ignorance is not benign. People often talk about feeling resistant to learn about or teach others about ACEs because it’s depressing, because there aren’t enough effective treatments for trauma and traumatic stress, for children or adults, as though not learning about trauma and ACEs has no negative consequence.
This is ludicrous.
The number of children, and adults, misdiagnosed, over medicated, shamed, blamed and stigmatized for being in pain or survival mode is alarming.
Having a context is crucial in and of itself.
Ignorance isn’t bliss. It’s not benign. Even in the absence of a “cure” for PTSD (which doesn’t exist) we need to get our hearts and minds wrapped around the real issues.
ACEs and the aftermath have huge personal and social impact.
While I hate that those impacted by trauma get a diagnosis of PTSD while those who cause it are rarely being treated, I am hopeful that the closer we examine the causes of childhood trauma the more we will have to address them directly – rather than treating only symptoms.
To me, PFE is an example of ACEs science making real changes in the lives of children and their families.
At the conference, Cooper asked attendees how many heard of ACEs? About 75% of us raised our hands. She asked how many had heard of ACEs several years ago. Few hands went up.
This is  incredible because it means more and more of us are ACE informed, trauma sensitive and armed with tools and education.
incredible because it means more and more of us are ACE informed, trauma sensitive and armed with tools and education.
It’s not that social policies and programs hoping to do a better job are new. However, not all walk the talk when it comes to being trauma-informed.
The PFE team made sure that the experiences of several trauma survivors who have or had involvement with DSS and/or mental health services were represented. More than one trauma survivor spoke about traumatic stress, foster care, therapy, family and individuals healing before, during and after being involved with services.
A young woman spoke about her family, experiences, foster care and therapy. Another woman spoke about being a mother having a child referred to DSS and their work, to heal as a family unit and to address the sexual abuse that impacted them both. I spoke about parenting with PTSD as an adult and being a kid with a social worker supervising visits with my biological father who had been abusive before he was absent.
We were talking with, as and about trauma from our experience. We weren’t token sob stories or present only to smile, sell and say thanks for all the services. We were there as mothers, activists, trauma survivors and also as people interested in improving policies and the system for others.
We were discussing ways to improve care, brainstorming and discussing system changes. And sometimes those with the most recent and intimate relationship with the system made the most brilliant suggestions. For example, the young woman who had recently been in foster care asked, during a panel presentation, about who gets trauma-informed education.
To date, trauma informed education is provided to therapists, social workers and foster and adoptive parents, and even to the executives at mental health insurance agencies, which everyone agreed was beneficial.
She wanted to know though if the education was being made available to the parents of the children in the system? Was it made available to the very people the kids would remain related to and maybe even be returning to?
It’s an excellent question. I wondered the same thing. Is training being offered to the parents who were abusive or neglectful and had maybe been abused and neglected as children?
So far, the PFE model doesn’t include trauma-informed parenting. That is not something routinely done or offered. However, more general parenting classes are reportedly being offered. I hope that’s true.
What I do know is that trauma-informed parenting was discussed and is being considered by thee PFE team as well. This is fantastic.
It made me wonder what my own early recovery from post-traumatic stress would have been like if ACEs education was made available to my entire family?
- What if expensive and often ineffective talk therapy had not been the standard treatment and there had been accessible workshops, educational seminars and family learning instead of or in addition to the “talking cure” that often made many of us feel worse?
- Those of us with high ACEs rarely come from parents without high ACEs.
- Those of us with high ACES generally come from parents who themselves have high ACEs.
- What if the way to break the intergenerational cycle of trauma is by making it so that all parents are trauma-informed?
- What if attachment 101 gets taught in in health classes, birthing classes or after delivery? Could attachment and trauma-informed parenting be available to all parents not just adoptive, foster or therapeutic parents?
- What if ACEs become mainstream conversation and all teens see the Paper Tigers movie in school?
I don’t have those answers but I’m more passionate and clear about the Parenting with ACEs group here at the ACEsConnection Network. And I’m clear that those of us with a trauma history must kee
p sharing our stories, experiences, ideas and strategies, personally a
 nd professionally, creatively and clinically.
nd professionally, creatively and clinically.
We can share stories, statistics and best practices. We can report on and brainstorm about what other individuals and organizations are doing. We can talk about the tools we wish we had or are creating to talk about, address and heal ACEs.
When stories and statistics are shared, side by side, change happens.
When all in the system are speaking to, for and about how the system does and doesn’t work, change happens.
It’s challenging at times. But when it comes to trauma and ACEs we can’t rush to resilience. We need to make communities more robust and stop asking more of our children and just let them be children.
I shared how the intimacy of having a baby often felt overwhelming to me at times. I didn’t share, that I was in fact, too terrified to get pregnant, be pregnant, give birth or breastfeed. But I did share how babies scared me by being needy, dependent, emotional, expressive and so physical. That’s healthy and normal, I know, but it freaked me out because I had survived adversity by ignoring my needs, body, feelings and sometimes checking out a little or a lot and using food, booze or compulsive busyness to cope.
Suddenly, as a mother, I had to be attentive, patient, present, affectionate, aware and half awake even while sleeping. Physical contact, to me, as a kid, had only negative associations. And all of a sudden I had to be in my own body in order to be present and responsive to my child. It was daunting, overwhelming and sometimes I felt smothered.
It was hard to admit that good mothering didn’t ooze out of me 24/7 naturally.
One woman who works with young mothers said, “I learned more in the last hour than I did in five years.” It’s not that she had never heard how parenting after childhood abuse could be triggering but she had not understood that even holding or hugging or what looked to her like positive interactions could be the triggers or why mothers sometimes seemed fearful or vacant with their own children.
I’d worried that if I co-slept with my toddler that in and of itself was intrusive or abusive. I worried if I hugged my daughter too much would she not be street smart or tough and wouldn’t be able to handle herself when threatened. So often, I taught my daughter to look out for danger but how rarely I taught her to appreciate and acknowledge and embrace safety, bounty, joy, play or curiosity. I didn’t do those things myself so how could I teach them? I was so intent on protecting and defending and reacting to a threatening world that I didn’t always remember to nurture or create a more positive world view or environment.
That’s not so easy to share either. And though it was terrifying at times to share so much that was gut deep and private, doing so helped me learn how deeply and how much people care about other people.
There are countless people who spend entire careers advocating for children and families. Many have ACEs. Many do not. I learned that there are far more people than I knew or imagined who want to make the world safer for all children. There are people who give years to work with, support and better understand ways to help others feel less alone.
And also, I was reminded of what I already know and sometimes forget… many of us are living with the impact of our own ACEs all the time and many are still doing daily battle to cope, function and get healthy.
People came up to me in private or wrote emails or comments on my website sharing their own stories of living with, in, through and with ACEs. Total strangers and I got teary eyed, held hands, exchanged knowing looks and sometimes laughed hard all in the same five-minute span. We talked about how hard it is to shop for cards on Mother’s or Father’s Day. We talked about the loving, triumphant moments when we realized our kids lives were far better than our own.
We celebrated too. We shared about the ways in which we had found, or failed to find, techniques to get through depression or anxiety or addiction. We talked about how an adult sometimes need to “mama our trauma” in ourselves and others, not only our children but of course, we need to be there front and center for them.
I can be cynical about “the system” and what can be done within it to improve things for people who are marginalized, vulnerable and have been wounded within families as well as society, in general.
But after this conference, I’m going to have to hang up and retire my more cynical self. I’m feeling almost hopeful.
You Matter Mantras
- Trauma sucks. You don't.
- Write to express not to impress.
- It's not trauma informed if it's not informed by trauma survivors.
- Breathing isn't optional.
You Are Invited Too & To:
- Heal Write Now on Facebook
- Parenting with ACEs at the ACEsConectionNetwork
- The #FacesOfPTSD campaign.
- When I'm not post-traumatically pissed or stressed I try to Twitter, Instagram & Pinterest.
Speak Your Mind