I’m sitting in the infusion center at Mass General in Boston. Soon, I’ll get a split dose of REGN4018 (meaning 10 mg. of infused today and another 10 mg. infused tomorrow and then if that goes well I’ll get a full dose of 150 mg. next week and then have another drug added in week 4). Today, because I’m about to start my second treatment. I’ll be inpatient as I was last week, when I got my first dose.
The first dose was only 1 mg. and if, like me, you thought “That’s basically nothing,” I can now say from experience it was not nothing.
It was not easy.
It was not just a baby dose.
It was a lot of a lot and a lot of it was awful.
It was intense.
I was knocked off my ass, and not in a slipped on a banana peel way, but in a struck by a plow going 50mph that didn’t see me in the snow and ran over me on the way back up the road. It was not only the going down and face planting that was rough, or being rolled over while already down. It was the fact that I stayed down longer than I would have liked, while shivering, sweating, and cold. By the time I could move it was not as I usually do. It was ugly crawling, hunched walking, and lots of grimacing and swears. I may have been counting one-Mississippi-two-Mississippi-three-Mississippi to try to either pass time or will it to come more quickly while waiting for the next hit of anti-nausea medicine, or pain relief, or fluids. I usually hate drugs and find the side effects of them equal to or worse than the benefits. This was NOT ONE OF THOSE TIMES. The side effects without medication were much worse.
I don’t know what exactly I expected but it wasn’t this. I guess we could say the first round exceeded my expectations and I only hope that the drug is delivering that same kick to my cancer as it did to me.
“Oh Cissy,” Dr. Penson said when he walked into my room at 9a.m. on Tuesday. I was wearing my winter scarf, had an eye mask on to block out the sun, and half my hair was sweat pasted to my head while the other half was sticking up and out. I’d brought make-up and a hair dryer as well as my computer because I had believed those things would be useful. Nope. I did not have the energy to even consider grooming never mind emailing, working, writing, or reading the news.
“Dr. Penson! That was a rough night. That was A LOT!” I said
“Didn’t I warn you well enough,?” he asked, and he had in fact warned to me expect to be flattened like the flu for two days, maybe more.
“But it was only 1mg, the baby beginner dose,” I said. “I felt nothing during the infusion. NOTHING AT ALL. And the nurses said I might feel nothing all night long. They said they thought I’d do well. Last night was not my idea of doing well,” I said.
I had a fever, vomiting, headache, and GI issues I told him and all of them came on fast. It was just one milligram – how on earth am I going to do 10 mg. next week two days in a row?
“The first can be the worst,” for some Dr. Penson said and the residents reiterated the same. They said it’s likely I’d feel the same after 10mg though maybe a bit worse or a bit better but that I would not feel ten times worse as I feared. I wanted to believe them and hoped they were telling me the truth but I worried it was just something said to get patients to return.
But I also reasoned that my first dose of chemo has also been my worst so maybe it was true. After my first round of chemo I had debilitating bone pain that nothing eased. It lasted two days but they were two long days. Luckily, I never had that symptom again. But it seemed counterintuitive to believe that ten times a dose, two days in a row, would not be worse.
My brother, Joe (broey to me) had been with me for 12 hours . We took the train into Boston together, and it was great to have his company. We talked, played cribbage, and ate crap food for the day. Though we live near each other and see each other several times a week, we’ve never spent twelve hours together without partners, kids, friends, or dogs so it was great to be with him. I loved spending time with him. He’s funny, easy going, and makes me laugh like few others. When we were debating over IV Benadryl or oral Benadryl, I requested oral because I didn’t want to sleep and drool on myself and IV Benadryl hits me hard.
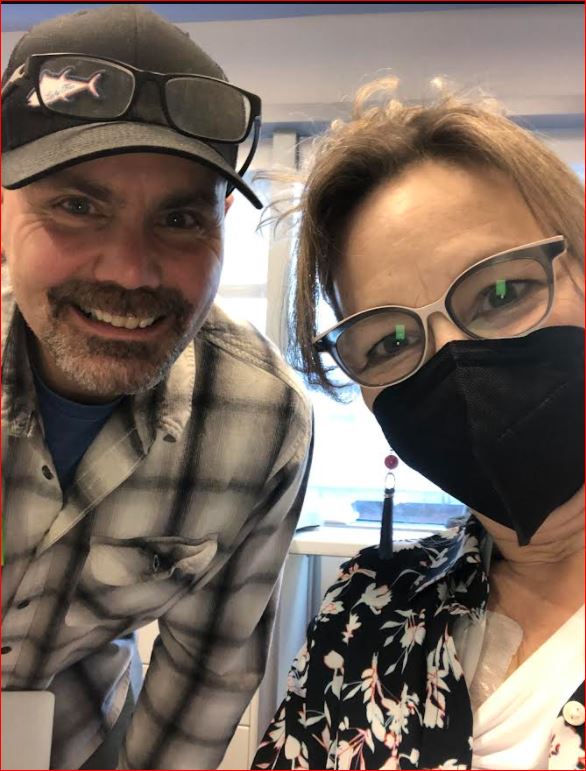
“Please give her the IV Benadryl,” he said to the nurse. “I hope she drools so I can take selfies with her,” he said.
He even waited til I was admitted to my room and was going to stay longer, but finally I said, “Go home.” There wasn’t much left to do or say and I thought I’d just get in my pj’s, maybe eat, read, and sleep.
That was not what happened.
He was not gone an hour and I went from feeling cold, to having the chills, to spiking a fever. I think I slept for several hours because I don’t remember anything from 7p.m. to midnight but I do remember heaving into a bucket starting at midnight and doing so off and on for the next five hours. The moment I got relief from vomiting, around 6 a.m., my GI system went into overdrive. Let’s just say it’s good that I had a private bathroom VERY CLOSE to my bed. My body’s reaction to REGN4018 was basically an urgent need to empty me of all my contents. I was turned inside out before I was discharged. The drug or the dehydration also seemed to make my heart pump faster as my heart rate jumped to 150 if I just sat up and left the bed. My oxygen levels and blood pressure both dropped day after and while it wasn’t dangerously low it’s the lowest it’s ever been for me (92% oxygen) and 95 over 55 for blood pressure. But as soon as I had some fluids both went up.
“Not everyone gets a fever,” Tina, the clinical trial nurse said when I came in the day after I was released for mandatory labs.
“Not everyone gets diarrhea. Not everyone vomits, and you got all three.” She thought I looked pale and out of breath and even the receptionist I’ve seen for two years noticed I wasn’t my usual self.
The doctor checked on me and ordered more fluids and I felt much better almost immediately. I let them know I’d spiked another fever at home which doesn’t always happen, and that I had more GI issues as well (though luckily the puking never returned).
“No wonder I’m dehydrated,” I said basically ever medical and non-medical person I came into contact with for the rest of the day.
Don’t get me wrong. My response was pretty normal and all fell into the “to be expected,” category. No one was alarmed or surprised by any of my symptoms and I’d been warned I might have “crushing pain,” where it “feels like you are kicked in the chest by a horse.” For that, and the abdominal pain some people get, IV Dilaudid is needed. In fact, I was told part of the reason I the clinical trial requires multiple hospital stays is because there’s no way (at least yet) which patients will have that). Plus, if one is in-patient, they can (and did) monitor one closely. My vitals were taken every half hour for several hours, then every hour for several more, and they were monitored a lot if my heart rate was high or my blood pressure or oxygen dropped. had a portable EKG I wore the whole time and labs were done regularly.
And, of course, my temperature was checked a lot to track my fevers.
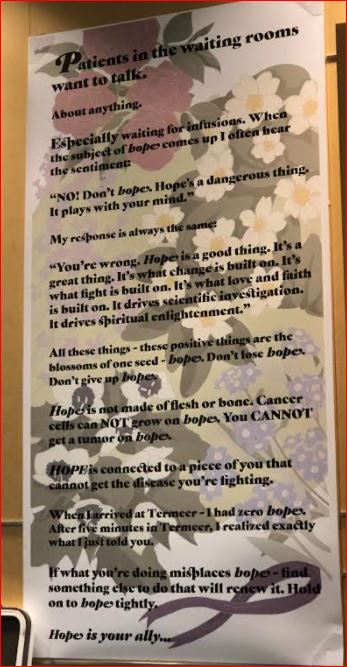
I felt well cared for but there are many unknowns in a clinical trial. And my go-to is always patients who have gone before me but this trial is so new those patients are not easy to find (I’m in the process of connecting with one thanks to my medical team). With most other treatments, I can hop online and meet others who have had the same or similar treatment, share tips and tricks about what helps or eases symptoms. I can’t do that as easily with this trial because it’s still so new. Part of the reason I’m blogging about this is so other patients who join this trial (or medical people interested in the patient perspective) can find something online.
I did a lot of guided imagery to help me stay calm and keep me from panicking about every symptom.
I hate and usually refuse painkillers but did take a half a Tramadol when I got home because the abdominal pain was making it hard to sleep or eat. At first I thought my stomach was wonky from vomiting or GI issues or the drug, but nothing I did (eat, get fluids, etc.) helped. The pain killer worked immediately and the stomach pain never returned. If I have pain again I will not wait to take a pain killer. My friends Heidi and Beth have frequently reminded me that the goal of the first month of this trial is just to get through it and not to tough it out on any level. I’ve been in treatment now for two and a half years and there are times I push back on or deny medications that seem excessive or don’t agree with me. But during this trial, I am just following orders and directions because it’s all so new and I don’t yet know what does or doesn’t help. I trust my doctor and he knows me well so that helps.
About the trial, as I understand it, (and my STEM daughter has helped demystify it for me), the first drug I’m getting, REGN4019 is a bispecific antibody that “tags” the cancer cells by attacking (attaching to) MUC16 (which is on the surface of epithelial cells). The presence of the first drugs, helps the immune system identify and fight the cancer which is important because ovarian cancer is expert at evading the immune system. This drug acts as a tag and also triggers the immune response. While this tagging the cells and stimulating the immune system is a good thing, it’s also tricky because they have to make sure not to trigger a cytokin release storm which can be really serious (and another reason patients have to go through a lot of tests to get into the trial and be admitted when we begin receiving it).
So, I started week 1 at 1 mg.
Week two is a split dose of 10mg one day and 10 gm. the next.
Dose 3 is a full 150 mg. and these are all done over several hours.
Assuming doses 1 to 3 go well, one dose is done outpatient. And then, another immunotherapy drug, Cemiplimab gets added in and for the first two times I’ll be inpatient again. If all of that goes well, I will be outpatient and get weekly infusions as long ad the drug is effective.
Supposedly, the side effects decrease as the body adjusts to the drug.
I believe in this trial because we need more options for platinum resistant patients like me who would very much like to continue living. There is at least one patient on the trial who has had one year NED (No Evidence of Disease, the best someone with recurrent ovarian cancer can hope for). She achieved this even after several prior lines of chemotherapy and that is a huge response.
“It’s kind of like the COVID vaccines,” one of the residents had explained to me. “We know what to expect and what can happen but we don’t know who is going to react, how long, or how much.” Some people get a fever and chills, some get a headache, some get nothing at all. They know the range of symptoms to watch for, and how to treat them, which is comforting, but it’s not fun to have what is essentially a sudden onset flu and stomach bug combined while away from home.
It knocked me out.
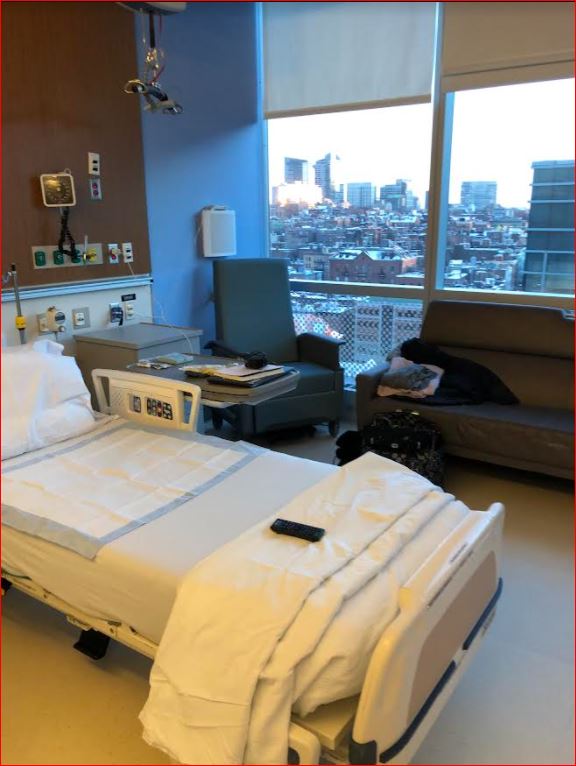
However, I felt exceptionally well taken care of the entire time. Despite feeling terrible, as someone on this clinical trial on the oncology floor meant I had my own room, and it was a huge room at that. It had a bed, couch, and a chair, a safe, a mini fridge and a bathroom. It even had some nice views of Boston. My brother said it was more of a hotel suite than a hospital room and he’s not wrong. The nurses checked on me so often I didn’t even need to use the call button. they were excellent as were the residents and the floor oncologist.
One nurse brought me ginger ale and rubbed my back while I was sick. One nurse brought me crackers and black coffee to ward off my caffeine withdrawal headache even if I couldn’t keep the coffee down for long. One nurse, said, every single time she left the room, “Is there anything you can think of that I can do for you? Is there any way I could help make you more comfortable.” That made me feel good each and every time she said it no matter how crummy I felt.
When you are scared, alone, and not feeling well, kindness is a type of well-being glue that makes the world hold together. It matters. It helps. It alleviates suffering. I don’t care if it’s called trauma-informed medicine or not. You can feel the difference when people are treating you like a human being and when they have curiosity and compassion and care about you. My oncologist had told many people I was a writer so when I was able to talk, they asked me about my writing, about my life at home, my daughter, and they shared stories and details about their lives as well. It helped.
This type of connection and kindness, especially when you can only have one visitor a day (Thanks COVID) matters.
While you know, intellectually, it’s likely you will eventually feel better, it is hard to trust that when you already feel weak, sick, and vulnerable. Because the treatment options for platinum resistance get limited, clinical trials are important. If we can extend time on non platinum drugs, and use drugs that don’t beat up the immune system, we can hopefully get more time. As the saying goes, “for something to change some thing has to change.” I’m hoping this drug is the change and that by participating in this trial I’m helping to make better options (and better dosing) possible for future patients.
I’m also aware that if I had little kids or had to work, I would not be able to do this trial. If I didn’t have love, support, and a car I couldn’t do this trial. If I didn’t have money to pay for the $20 round trip (if taking commuter rail & T or paying for parking) I couldn’t do this trial. For this trial, I have to come in once for a one-to-night overnight and then two other times every week for lab draws. Basically, I’m here five days a week for five weeks. I’m on disability and no longer work, and my daughter is 19 and living at college, so I can do this but others who could benefit as well can’t.
Not everyone has equal access to clinical trials or this level of care the ability to try a new treatment. I worry that it’s not only a health equity issue, but also skews the results because it’s a specific patient population that can participate. So, when I complain about how crappy I feel, I try to keep in mind that I’m lucky to even be in this trial (it had a waiting list).
While last week was one of the harder weeks I’ve had since diagnosed with ovarian cancer, it was bearable because of the outpouring of love, care, tenderness, and practical support I received. At first, I felt knocked over by a plow, but by the end of the week I felt like 100 people come to help me get in the house, get warmed up, fed, and helped me recover.
It’s been incredible and we’re talking about love, care, and tenderness that have lasted years. .
I’ve gone through two rounds of a chemo, another clinical trial for maintenance drugs hoping to keep the cancer at bay, and I’ve had one major surgery and a few minor procedures. I’ve not been near as present, attentive, and there for my loved ones in the past two and a half years as I would like and they have loved me anyway. The only reason I got through the last week was because of friends, family, and all the help and love. I felt carried and calmed by love.
I also had a few insights and realizations I’d like to share and hope that no one else needs to get cancer to learn these lessons:
Help helps.
It feels good to feel good.
It feels bad to feel bad.
Support supports.
Sometimes, it’s a luxury to shower without exhaustion or do a flight of stairs without breaks or being short of breath.
Rest requires wellness (even with a long-term spiritual practice). What I mean is that it’s hard to rest when puking, hard to “chill” when in pain, and next to impossible not to get cranky when depleted, dehydrated, and mega-dosed with a whole lot of drugs. I guess I didn’t realize how much of my personality is based on feeling fairly decent. I have new respect for people with chronic pain.
It’s impossible to capture all the kindness, but in addition to countless texts, calls, FaceTimes, and in person visits, people have sent cards, made homemade meals, and driven a long way to get them to me. People have brought me fluids and flowers, smoothies, and ginger tea. I fear forgetting people but I have to shout out thank you’s to a few people and also hope it helps give you ideas of what can help people dealing with cancer treatment.
My aunt had flowers and comfort foods and beverages delivered to my house. She checked in on my constantly and reminded me to turn off my phone and sleep when I felt lousy. My sister arranged rides home from the hospital for the first six weeks of the trial and drove a long way to visited me at MGH when I was in the hospital. She also helped me prepare the house before my first admission.
My cousin Jenny made me homemade soup and brought tons of food. She visited for hours and drove me to my first lab appointment. She love bombed me with videos of her son laughing and and being adorable. And she arranged a meal train which I at first declined. She said, “You have to let people do something because we feel helpless. Please let us do this.” I did and I had no idea how much I’d need and appreciate it. My friend Deb took me to get reflexology and we walked, played with the dogs, and talked.

Heidi came to work at my house just to be around and available and also treated me to a pedicure (first in two and a half years). She always makes me bone broth, brings me fluids, calls, and reminds me to reach out at any hour. After she left, there was a note on my chalkboard that said, “I love your face,” and I’ll never erase it. She texted me to say, “I wish you the strength of 10 women going into the next treatment,” and I had had the love and support of at least 10 people who are letting me borrow their strength, faith, and optimism when I’m just in head down and survive this mode. It’s humbling, touching, and I’m so appreciative. I’ve never talked so much about my body, aches, pains, and issues before and feel bad that many conversations are boring or one-sided.
Beth visited me at the hospital, called, texted, loved me up. She brought me home from the hospital, fed me dinner, and slept over to make sure I was o.k. She brought me pistachio nuts and crackers and mints. She calls me all the time. She takes notes and tracks my symptoms. She never makes me feel like a burden. And when I was annoyed that my cancer spread to more lymph nodes and that some of my lymph nodes got even bigger, she said, “Those lymph nodes are working so hard. They’ve kept things from spreading more and kept the cancer in check but it’s time to get them some support.” I love her perspective. It helped me appreciate how hard my lymphatic system has worked against a cruel enemy.
My aunt Diane sends me inspirational messages often, and sent me PJs to wear at the hospital as well as sent water bottles and countless gifts.
My cousin Katie and her husband Evan dropped by and made enough food for me to eat four meals and it was so fun I forgot I’d ever been sick. It was lovely to sit in the living room and enjoy each other.
The challenges have been intense, and I kept telling Beth, “My body is the boss. I’m my body’s bitch.” I felt like all of my energy was going into keeping food down, keeping up with fluids, monitoring my oxygen, heart rate, and breathing. It felt like all I talked about last week was what hurt, where, and how much.
Still, people have not only tolerated me they have loved me fiercely and helped transport me, feed me, and lighten the load. They have reminded me of what I have done for them in the past few years even when it feels like nothing. This trial has been a trial not just for me but for all who love me.
P.S. Lesson Learned
“You’re so on the borderline,” the nurse said and seemed to be pushing for me to stay an extra night. She wanted to make sure the fluid wasn’t artificially raising my blood pressure and lowering my heart rate. She didn’t want me to have issues at home where I’d not have access to the medical team or things like fluids. The resident kept saying I could go home, was fine, and I kept dreaming of sleeping in my own bed. He felt confident about it because I was required to return for labs the next day and knew I’d been seen within 24 hours.
Yet, when I got home I was in rough shape. I had abdominal pain, GI issues, and spiked a fever. I was sharing all of this with my friend Karen, who is ICU nurse who stopped by with soup, flowers, and treats. She asked me, “Who spent more time with you? Was it the nurse or the resident. If you were my patient I wouldn’t have wanted you to go home either.” The resident had spent ten minutes with me. The nurse saw spent hours and hours with me and saw me at my worst. She was there when I vomiting, feverish, and my blood pressure and oxygen levels went down. She saw me struggling to eat anything at all or even to get water down. From now on, I will defer to the nurse when it comes to if and when I will be discharged. I respected my resident but I now know I was not really ready to go home though I wanted to sleep in my own bed.
P.P.S. I will get a scan in three weeks to see how the cancer is responding to the drug. If I respond to the drugs, I’ll be on this weekly regimen as long as I keep responding. I think after one year, one can have one week off a month to travel, etc. So, fingers crossed that the side effects decrease while the effectiveness at fighting cancer increases. Several people told me that fevers and reactions are good because it indicates the immune system is engaged and activated. While it doesn’t feel good, I try to keep this in mind and imagine that the symptoms are because my immune system is clearing cancer from my body. While no one guarantees that all with symptoms will have a good response, or that those without symptoms will not, the trend seems to suggest that a robust response is positive. I sure hope that’s the case.
You Matter Mantras
- Trauma sucks. You don't.
- Write to express not to impress.
- It's not trauma informed if it's not informed by trauma survivors.
- Breathing isn't optional.
You Are Invited Too & To:
- Heal Write Now on Facebook
- Parenting with ACEs at the ACEsConectionNetwork
- The #FacesOfPTSD campaign.
- When I'm not post-traumatically pissed or stressed I try to Twitter, Instagram & Pinterest.
Love you. Hate the side effects. Love your writing. Cannot wait for you to be free and clear. Hugs. Loving you madly from afar.
🦋❤️🦋
Thank you, Carey! I so appreciate you and thank you for your constant love and care even when I’m lame about calling!
Warmly,
Cis
Like all your writing, it shouts! Your words grab me and hold me at full attention to the end. You don’t hold back. You let me know and I want to know. This trial is so hard. But you are in it and doing it. Hang on. Hope the 10 mg. dose runs over the cancer cells like a snow plow.
Thank you, Margaret! I really appreciate it and round 2, both 10mg doses were much easier than round one and I’ll write about that as well. Thanks for reading and for caring!!!
Hope you are well!!
Unbelievable, Christine. Thanks for sharing your experiences with the world. Wishing you the warmest, bestest.