Warning: This post was written by a weary, anemic, fever-brained writer.
This trial is brutal. When I go in for treatment on Tuesday it will have been exactly one month and it is fair to say it has been the hardest month of my life.
Would I have done this trial if I knew exactly how hard it would be? Probably, because my other choices are all pretty crappy and limited. Still, do I wish I had known exactly how hard it was going to be? Yes. It’s not only been hard on me but my friends and family who have supported me SO MUCH and are the only reason I’m still functioning.

I don’t want to sound negative but I do want to be honest because I know I appreciate honesty. It’s very hard to find anything online about people who are in this trial and what we are experiencing which is why I’m determined to blog and share at least one patient perspective. I’ve not found anyone online who has done or is doing this trial and the one patient my oncologist got permission to her number with me and I have not connected. There needs to be more online and available to other patients and families.
This trial is intense and exhausting. And as I say this I am aware that this is the first time I’ve had weekly treatments, and treatments that require in-patient hospitalizations for 1 to 2 nights for most of the first six weeks. This happens to others getting cancer treatment but it’s a new experience for me.

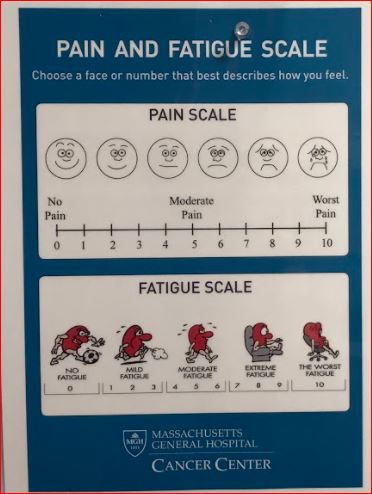
I had no idea how taxing and grueling the schedule and requirements of the trial would be. Because the trial doesn’t just require in-patient hospital stays, and come with severe side effects, but most weeks, requires going to Boston twice a week to give labs (or get fluids if need be). It requires monthly eye exams, and twice a month echocardiograms as well as once every six week CTs. Again, all of this might not feel so burdensome but I’ve not had one day on this trial without a fever (or a high temp for me) and without vomiting (which I was lucky not to experience hardly at all during chemo rounds 1 or 2). But getting motivated to do anything when it feels like you have the flu feels hard.
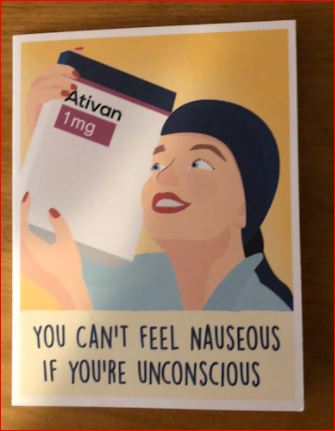
This card made me laugh because it’s funny. There’s that. but also because one of the nurses at the infusion center saw me pacing one day and asked if I wanted Ativan which I declined. I thought it was only for anxiety and not also for nausea and rigors (uncontrolled shaking as temp climbs and fever starts). Well, an hour after he asked if I wanted Ativan, I was throwing up and had rigors for the first and I hope only time in my life.

In addition, while I’ve always been pleased to be able to be independent (and am walking distance from a commuter rail and driving distance to the T), there are many days pre or post treatment I’ve not been well enough to walk or do public transportation. It’s been humbling to feel so weak and needy. It’s hard to have to rely on my loved ones.
Plus, transportation costs aren’t cheap, especially with gas prices going up, and these expenses are not covered by this particular trial (some trials do cover travel expenses). The fact that this trial doesn’t cover this when it requires at least three times a week visits for the first six weeks surprises me. However, last week I did get access to the Ride which in greater Boston at least provides affordable rides to and from MGH (and other places) for people with disabilities. The cost is about 1/10th the cost of Uber or Lyft. This has been extremely helpful and was coordinated by the Social Service department at MGH which meant minimal paperwork for me.

However, it’s still a lot of coming and having to leave the house when feeling terrible. There are extra trips for things like blood transfusions (which I had last week), for infections or complications which require procedures or unplanned visits. There are changes in schedule, so even though my dear sister tried to arrange a pick up for me after every infusion, and created a calendar so all know my schedule, the schedule changes so much it’s not accurate or easy for me or others to plan.
For example, last week I was supposed to have an infusion on Monday, and it was to be my first one at full-dose as an out-patient but, when the labs returned my liver counts had increase by seven and a half times and treatment was put on hold. It was not clear, for days, if it was from the drug or the massive amounts of Tylenol and anti-nausea meds or how quickly they would return to within limits for treatment. It’s been a learning curve figuring out how to manage daily nausea and temps. Luckily the counts came down after four days off the Tylenol.
I don’t mean to complain or be extra but I do want people who are considering this trial to know it’s consuming. It would be impossible to do if one has a job, young children, or really any caretaking or other responsibilities. I’ve barely been able to keep up with anything other than the trial and slouching on the couch and feeding the animals and that is with a ridiculous amount of help, support. I have a twice-a-week meal train arranged by my cousin Jenny, and endless rides, calls, texts, and TLC from my family and friends who visit, who drive me, who do errands, who listen to me vent, cry, and keep asking how I’m doing, and act like it’s interesting or new even though I’m basically saying the same thing every damn day.

I think about that every time I need a pill and it makes me laugh every time.
This trial is impossible without a serious and heavy-duty and incredible support system. This means that there are many people who do not have access to this trial because they can’t miss work, because they care for kids, parents, (or both). For people who are further away from a huge medical center than I am this would be even more cumbersome and time-consuming. The labs and tests can’t be outsourced or done at local clinics or hospitals.
The phone calls, texts, schedule changes all take up a lot of time as well and all feel infinitely harder when feeling flu-like. Basically, I have spent the last month feeling like many felt the day after getting the COVID shot who got fever, chills, headache, as well as a having a stomach bug combined and severe anemia to boot.
I have been less great at joy-stalking than I expected. I have have infinitely more empathy for people with chronic conditions. It’s hard not to feel worn down when worn down. It’s hard to be present and show up for others when most days are about trying to keep temperature managed, body from getting dehydrated, and getting enough calories in to keep up the stamina to keep going. Never ever in my entire life has it been hard for me to eat or rest. I could be a professional eater or rest queen so I don’t even know this agitated and force-feeding version of myself. Usually I can eat like I’m eating for five. Now, it’s hard to eat the equivalent of two meals.


Also, next week I’ll have my first scan and I am hopeful about that and hoping to be screaming and positive and saying, “it is all worth it” because I have felt the lymph nodes in my neck, chest area, and armpit shrink. If I am able to stop progression and even reverse some of it – I will be happy. I remind myself of this often to keep going and so far, there have only been two days when I have thought, “I just can’t do this anymore.” Luckily, on those days I had people love me up and help me out and remind me that anyone with a fever for an extended time gets worn out and is less perky than usual.
And it’s not all been hell. At all.

My uncle has also been wonderful and has driven my back from MGH more than once. But it’s not just the errands and the rides, the amazing food and beverages, it’s the LOVE. I feel it deeply and all and much more than I’ve felt it in the past. I am so grateful to be able to feel all the love,
support, compassion, tender, care, and bounty.
I will write more about specific moments, amazing interactions with my loved ones and friends and how we have laughed, talked, had heart to hearts. There’s too many examples to name them all but my cousin Jeff has been sending me songs almost daily and it’s been fun to think about something other than what hurts.
My friend Heidi came with me to an appointment but it was more than that. I had hit my wall and wanted to quit the trial. She let me vent, came to my house (with coffee), drove me to my appointment and even had a blanket ready for the car ride. Then, we got dinner on the way home. Who and how I was when I woke up that day and who and I how I was when I went to bed were completely different. She pasted, glued, hot gunned, stapled and loved me so hard I was put back together. I don’t know what I would have done without her love, support, and help. These are the types of things that make me wonder how I will ever be able to fully appreciate, thank, and repay my loved ones. It also makes me grateful that I have such amazing friends and family.
My family and all of my friends have been providing non-stop food, love, rides, and care. I am completely humbled and grateful.

people are making me food, driving to deliver it, and / or getting gift certificates in my local area so I can order food. It’s been a HUGE help though sometimes I can’t eat all the food I get. It’s strange not to eat like I’m eating for five, but these days that’s where I’m at.
And I’ve had amazing nurses at the infusion center and when in-patient and they have all, without exception, been exceptional and caring beyond just making sure I’m a body that doesn’t croak on their watch. I’ve met wonderful people, learned about their lives, families, hobbies, interests, and how they got into medicine. We’ve talked cancer, clinical trials, and the pros and cons of alternative treatments. They have shared with me what it is like to work on an oncology floor.
And my oncologist, and the clinical nurses, coordinators, nurses and nurse practitioners have all been extremely kind, caring, responsive. It all has made this trial bearable and can’t be ignored. I know not all have this much love, support, and quality medical care, and I know that even with all of it it has still been absolutely brutal.

My fervent wish is that someday the minimum effective dose will be the goal when giving patients pills as opposed to the current standard which is the maximum tolerated dose. The dose escalation in my trial felt intense. I went from 1 mg (week one), to 10 mg. two days in a row (week two) to 150 mg (week three). It has been scary to face these increases and it’s not just me that has questioned the rapid escalation but also the infusion team and some of the medical staff who care for me in-patient. However, they have been told, as I have been told, that things do get easier week over week for most patients (including me) that’s mostly been true. Things are far from EASY but they do get easier (less low and scary blood pressure, less high heart rates, lower fevers and less hours of vomiting). But still, four weeks in there’s not been a full feel-good day. There are just days that feel not so bad or less bad. Again, this may be the pattern for anyone getting weekly treatment and not a result only of being in this trial.
Also, while me team always asks how I am, what I am experiencing (symptom-wise) and is responsive when I need fluids, bloods, etc. I don’t think there are reported outcomes or forms or formal surveys of patients. While I’m sure the medical team conveys what we are experiencing, I do not understand why patient reports wouldn’t be beneficial as well. As a patient, I can talk to my nurse or my team but there’s nothing in the study that asks about my quality of life is, how difficult or burdensome or grueling the drugs are or even how challenging the schedule can be. There are patient advocates working to include patient experiences more formally and I support them in doing so.
It’s actually shocking to me that patient input (provided by the patient) isn’t considered crucial to the drug makers as well as to the medical teams caring for us. It’s like if only Apple got to say how IPhones work for consumers, and consumers never got to talk about software bugs, high costs, or opinions on product effectiveness. It’s not exactly an unbiased system.
In my opinion, it’s not patient-centered care if it doesn’t center the patient.
Currently, trials center the protocol and not the people on them. This is one of the hardest aspects of being in a clinical trial.
Hopefully, next week, I’ll be writing about how much my lymph nodes are shrinking and how all the pain is worth it and I still am happy to participate in a trial that offers some hope and change as the standard of care in ovarian cancer remains the standard of fail for the majority of us. I’d like to be part of something that makes a difference for others, and of course, I hope it makes a difference in my lifespan as well.
But this week, I can only share that it’s been an epic trial and I am one lucky woman because I have others who are walking with me, caring for and about me, nurturing, tending to, and caring about me even though I have so little to give back.

While I have never felt weaker in my life or in the two and a half years I’ve been dealing with advanced cancer, I can say that I have never felt so loved. Sebane Selassie distinguishes health and wellness and says we can have a sense of wellness even when ill (and can have a sense of un-wellness even when healthy). That speaks to my soul and to where I am emotionally and spiritually (most days) despite the challenges. I know she has had to deal with several recurrences of her stage 4 metastatic breast cancer and so I follow her posts, newsletters, and social media closely and am inspired by her approach to mindfulness while metastatic.
P.S. A few tips I have learned so far:
It’s helpful to bring your own coffee and snacks and food to in-patient stays as the only food available on demand is saltines or graham crackers. If, like me, you wake up starving at 2a.m. it’s nice to have something familiar and hearty. And, if you are in a bad place when the food from the hospital comes, it’s nice to know you don’t have to wait five to six hours to eat or drink more than crackers or water.
It’s helpful to bring cozy pjs and a soft blanket because hospital blankets are basically white sheets.
It’s nice to have visitors even when you think you are fine and don’t need them and don’t want to bug them or mess with their job and family schedule because it never fails to lift the spirits.
It’s great to have guided imagery or podcasts or dumb TV on when you need to get out of your head and symptoms. It doesn’t always help tons but it can get help give one a tiny bit of distance from the pain.
It’s o.k. to tell your loved ones how hard it is though it can feel like being negative or whining.
It’s good to ask for help before you have hit the wall. I’ve failed at this twice but am hoping I’m better at reaching out next time. I can go from, “I’m fine. This is fine. I got this. I got this,” to “Holy Hell I can’t cope and what did I get myself into and what torture did I sign myself up for and how do I get out?” in a few hours.
When your friends or family say call or go to the doctor, call or go to the doctor. They sometimes can see you are weaker or declining when you can’t because the changes feel incremental when you are living them.
When you really are having trouble eating anything at all, it’s o.k. to get down whatever you can even if it’s ice cream or pickles or hash browns or things you didn’t even know you liked.
FINAL NOTE:
P.S. I have had two fever-free days and two days without being sick to my stomach. My appetite is better. My energy is better. My mood is better. I almost deleted this entire post. However, this is the truth of how I felt when completely bone-tired and worn down so I’m going to keep this posted just to give an idea of how things can feel at least some of the time.
You Matter Mantras
- Trauma sucks. You don't.
- Write to express not to impress.
- It's not trauma informed if it's not informed by trauma survivors.
- Breathing isn't optional.
You Are Invited Too & To:
- Heal Write Now on Facebook
- Parenting with ACEs at the ACEsConectionNetwork
- The #FacesOfPTSD campaign.
- When I'm not post-traumatically pissed or stressed I try to Twitter, Instagram & Pinterest.
Your writing has given me insight into both your physical and emotional state. Your attitude continues to inspire and humble me. You are amazingly brave and admirable ❤️
You are amazingly kind and generous, Ellen!
Love, Cis
What a beautiful and honest thing to share Cissy…you, going through something hard and painful and uncertain, trying to provide hope both for yourself and your family, but others who may walk your path. I’m so glad you didn’t delete it. And I love you for having the courage and strength to share it.
Thank you, Brenda:
I know I always want real-life reports and experiences, even when hard. But, it’s hard to remember that others might appreciate it as well. Thanks for the affirmation and the support. Warmly, Cissy
I have been waiting for your update. And knew from the wait that week 2, 3 and 4 must have been brutal. And brutal describes it. Your courage to do this is awesome and more than just “some.” Thank you for putting your perspective at the center. When you write you teach me what this cancer thing is doing to you. You refuse it. A trail.
Thank you Margaret!!!
I am learning so much and I have been trying to think of artistic things to do with things like my PleurX bottles and all the hospital bracelets the way we did with the body language exhibit.
I’m better this week (week 5) and will be writing about that soon. I miss you (and Ruby)!
Love, Cis
I love and hate this all at once. The pictures of you and Beth, momma and baby giraffes and sunsets are amazing.
Hearing you endure the pain and exhaustion day after day breaks my heart.
Hearing about all the ways friends and family are being allowed to love you warms my heart. I know accepting help, much less asking for it, requires the kind of strength your red blood cells just haven’t had lately. I’m wicked proud of you.
Thanks for all the love, support, and witnessing Heidi. I don’t know how I would do this without you and I’m grateful I don’t have to know. I wish I took pictures when you were here. NEXT TIME!!!
Love, Cis
Cis,
I am continually amazed at your strength, attitude and ability to share so much for others when you are going thru such an intense, emotional and weary journey! YOU are amazing! YOU are strength, beauty and love divine!!! Sending you so much love and you are always in my daily prayers. Praying for you so hard!!!
Much love my friend,
Terri
Terri:
What a kind and uplifting comment to read! THANK YOU!!! Truly, it makes me feel great. And it also helps me to think that sharing might benefit others who do this trial or know someone who does.
Thank you for the love and the prayers. I’ve been blessed with so much kindness and caring and it’s magic and medicinal and helpful!!! So thank you!
Warmly,
Cis