It’s spring in New England, but trauma survivors are still left out in the cold without hats, help, or hope.
The cause is a man-made crisis among the Trauma Center leadership who seem more concerned about who gets to fire whom over allegations of sexual harassment and workplace bullying than the cause of complaints or the needs of survivors.
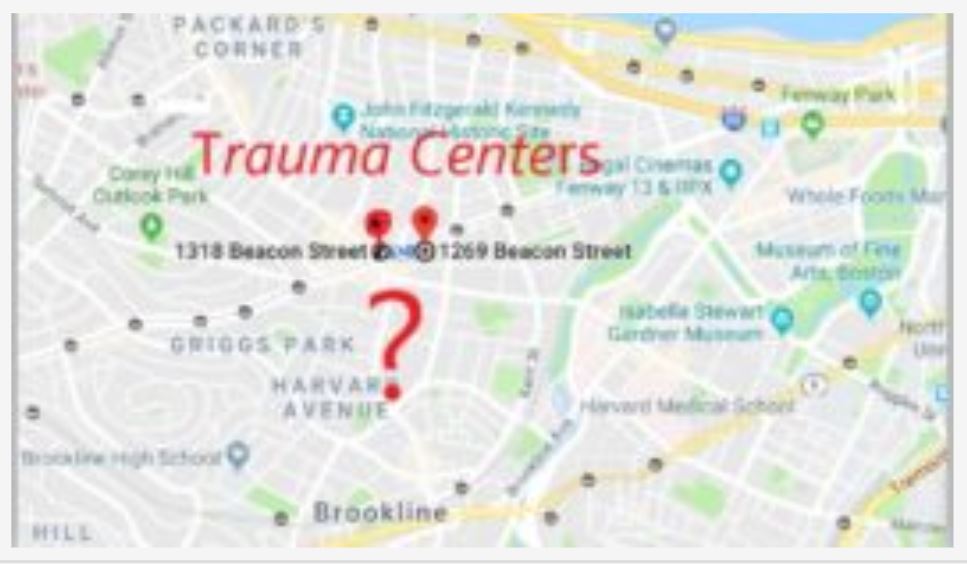
The trauma center is split in two. We have trauma center one (at Justice Resource Institute) www.traumacenter.org, and trauma center two, (of the Trauma Research Foundation), www.traumacenter.net. They share almost identical names, websites, and addresses.
Trauma Center 1 is at 1269 Beacon Street. Trauma Center 2 is at 1318 Beacon Street.
Instead of twice the support, we have less. Trauma Center 1 (at JRI) isn’t offering clinical services to individuals until September, per their website, which I’ve been tracking for months.

Trauma Center 2’s website says clinical services will be available in the Spring of 2019 but doesn’t respond to email inquiries about how and where to access them. While it’s hosting the annual trauma conference, continuing to run the trauma center certificate program, if you’re a trauma survivor in crisis, you’re out of luck.
Both trauma centers have fundraising campaigns and are accepting donations (no wait times, there).
This prolonged crisis is the opposite of what Mayor Marty Walsh meant when he implored the nation to look to Boston as an example of bridging differences to care for people in his State of the City address. We deserve leaders who manage and mediate rather than manufacture or magnify conflict.
As a survivor who has sought help from the Trauma Center at JRI, I’m furious and frightened. This situation is potentially catastrophic and triggering for many of us.
I remember my first anxiety attack. I woke at dawn feeling as though fireworks of heat and adrenaline were exploding in my body. I oscillated between hot, cold, nauseous, wired, and exhausted as if a wildfire were spreading beneath my skin. It was hard to think or talk. I felt as if I were dying or losing my mind and feared I’d end up battling alcoholism, homelessness, and violence, like my father – a veteran of Vietnam and his crappy childhood. I felt desperate and overwhelmed. I didn’t understand at the time what post-traumatic stress was. I know now,
When post-traumatically stressed, it can be hard to breathe, sleep, eat, cope, or function. In terror and desperation, survivors can lose tempers, jobs, and lives. The general public may not understand how life-altering and life-threatening traumatic stress can be. The Trauma Centers (.org or .net) can’t say the same. They know the importance of being trauma-informed, trauma-sensitive, and trauma-responsive. They know how common trauma and traumatic stress are. They know how central support and safety are to all survivors, at all ages and stages no matter the cause of traumatic stress symptoms whether they resolve quickly, are intermittent, or last a lifetime.
After all, the former executive director of the old and new trauma center, is the same, Bessel van der Kolk, author of what many consider the bible of developmental trauma and post-traumatic stress treatment: The Body Keeps Score: Brain, Mind, and Body in the Healing of Trauma. The backstory about how Andy Pond of JRI fired him is relevant but secondary to the crisis for survivors and staff caused by the battling of these men.
Each has claimed to be less at fault and more concerned about survivors, staffers, and the trauma center. To me, they appear to share responsibility for failing all three. Boston, once known as the place to go for innovative, world-class treatment options for traumatic stress, has two trauma centers that lack the skill, will, or ability to prioritize survivors – for more than a year.
The leaders of both trauma centers have been too engrossed in a nasty, public, and prolonged professional split to notice the survivors they’ve abandoned and staffers they’ve put in the middle.
The current situation at the Trauma Center/s is potentially catastrophic.
I’m no longer in crisis but I will never forget that every minute others are and that any of us could be as well. People in crisis and seeking help deserve more than a long list of referrals for other places to call and to be told to check back later, and later, and later.
The anniversary of the bombing at the Boston marathon is Monday. We know, trauma happens suddenly, to children and adults, in public as well as private spaces. We know, from recent news reports, that traumatic stress can impact survivors and families for months, years, and decades.
In the last month, we’ve lost three different people to death by suicide – following tragic mass shootings, and those are just the stories that made front page news. Every day, people die of suicide. While social media memes advise hanging on and reaching out, those words are meaningless if there’s little support available or affordable when people do so. This is precisely what mental health parity laws are supposed to protect us from.
Imagine having a life-threatening cardiac event and being given a list of general practitioner because the cardiologists are too overwhelmed with legal and professional conflicts? Picture having an asthma attack, finding the breath to call for help, and being told to come back – in six months to a year? This would be unacceptable and would make front page news.
The “state” of mental health parity in Massachusetts has a long way to go.
I hope this crisis creates an opportunity for trauma-informed systems change and creative collaborations among communities and the Commonwealth. Might our leaders intervene?
Can we review and revamp how mental health funds get allocated and administered—and to whom? Where are the citizen advisory boards? Who is monitoring the situation locally?
Can we insist that trauma center leadership be more representative of those diagnosed most with post-traumatic stress disorder and who have the most adverse childhood experiences – namely, people of color, the poor, females, those with have disabilities, and identify as LGBTQ? It’s not what we’ve had and here’s where we are.
Survivors shouldn’t have to educate trauma centers on what’s damaging, dangerous, and triggering. Trauma centers should be places we can count on for sanctuary, and solidarity following unimaginable horrors, heartbreaks, and violence. They should hold us as we grieve, get steady, and heal.
The same city known as Boston Strong has been Boston Wronged by our Boston-based trauma center/s.
Note: Blog image of glasses came from artwork done by Margaret Bellafiore & Cissy White for Mobius interactive installation entitled Body Language.

9
You Matter Mantras
- Trauma sucks. You don't.
- Write to express not to impress.
- It's not trauma informed if it's not informed by trauma survivors.
- Breathing isn't optional.
You Are Invited Too & To:
- Heal Write Now on Facebook
- Parenting with ACEs at the ACEsConectionNetwork
- The #FacesOfPTSD campaign.
- When I'm not post-traumatically pissed or stressed I try to Twitter, Instagram & Pinterest.
Speak Your Mind